From the beginning and now for a long time, opioid analgesics were reserved for a few select conditions, such as surgery, cancer and other terminal illnesses. The marketing tactics from the drug makers and FDA approvals allowed and encouraged doctors to prescribe opioids with much more ease for many pain related conditions.
It is not uncommon to anyone that this liberal prescribing of opioid medications to patients suffering from pain and pain related conditions has led to one of the largest crises in US health history, with wide implications in many other areas. Economists and politicians alike are involved in analyzing this epidemic and trying to find solutions for remedy.
Obviously, at the center of attention in dealing with this epidemic are the prescribers – pain management specialists. As they were initially seen as the main cause of this epidemic, they are now expected to be the solution finders. If things were only that simple!
However, some of the major challenges faced when prescribing oral opioid therapy, such as addiction, digestive problems, behavioral issues, etc., may be spared by using pharmaceutical compounding.
Pain management doctors that want to help their patients experiencing pain using the safest and effective customized treatment solutions, are already prescribing compounded medications.
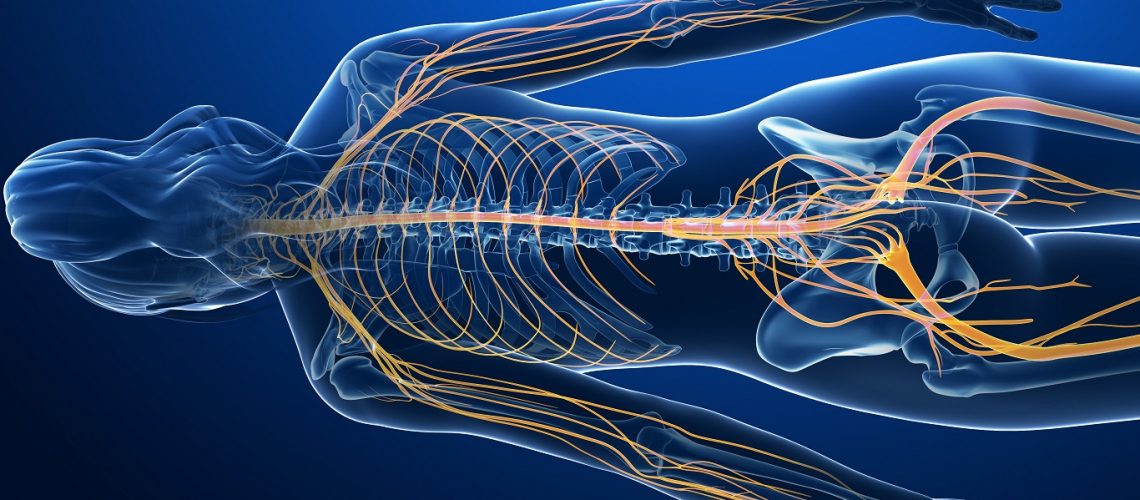
One preferred route of administration, heavily studied in the last years, particularly for pain management, is transdermal administration. Transdermal compounded medications are patient-specific and customizable. They can include various active pharmaceutical ingredients (API’s) in many dosage strengths to be delivered together in one application. Combined API’s in transdermal preparations may include non-traditional pain management options that can help maximize therapeutic effects of the medications. This is achieved through the additive or synergistic properties of the medications, without the need to increase the strengths of the core drugs.
Because pain has different origins and comes in diverse types, combining multiple classes of drugs with various mechanisms of action can be very beneficial when customizing the treatment.
There are algorithms created by large groups of pain management practitioners that offer guidelines in selecting the API’s, their strengths, the combinations and their corresponding indications.
Transdermal delivery of compounded pain medications has reduced adverse effects compared with oral opioid therapy. This increases patient compliance and minimizes exposure to potential abuse and addiction. The use of compounded transdermal pain medications may help healthcare practitioners effectively treat their patients while avoiding the use of addictive oral medications.
If you are not using pharmaceutical compounding in your practice and want to help your patients avoid the possibility of opioid addiction, now is the time to select and contact a reliable compounding pharmacy.
Let your selection be HALDEY Pharmaceutical Compounding. Talk to any of HALDEY’s experienced compounding pharmacists for any questions you may have related to customized transdermal pain management medication. Give us a call today to learn more about compounding.
References:
Peppin JF, Albrecht PJ, Argoff C, et al.: Skin matters: A review of topical treatments for chronic pain. Part one: Skin physiology and delivery systems. Pain Ther. 2015; 4(1): 17-32.
The role of transdermal compounding in opioid safety Caitlin V. Bucher, PharmD, A.J. Day, PharmD, Maria Carvalho, PhD
Bassani AS, Banov D, Phan H: Characterization of the percutaneous absorption of ketoprofen using the Franz skin finite dose model. Postgrad Med. 2016; 128(2): 262-267.
Dowell D, Haegerich TM, Chou R: CDC Guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016; 315(15): 1624-1645.
Bassani AS, Banov D: Evaluation of the percutaneous absorption of ketamine HCl, gabapentin, clonidine HCl, and baclofen, in compounded transdermal pain formulations, using the Franz finite dose model. Pain Med. 2016; 17(2): 230-238.
Vowles KE, McEntee ML, Julnes PS, et al.: Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain. 2015; 156(4): 569-576.
Jorge LL, Feres CC, Teles VEP: Topical preparations for pain relief: Efficacy and patient adherence. J Pain Res. 2011; 4: 11-24.
SAMHSA (Substance Abuse and Mental Health Services Administration). Managing chronic pain in adults with or in recovery from substance use disorders. TIP (Treatment Improvement Protocol) Series 2012, 54, Report No: (SMA) 12-4671, Rockville (MD).