- We all know about women and menopause.
- But do we know that men go through “the change” as well, as they age? And that the “change” stage is called andropause?
- The answer is: “yes”, “no”, “maybe”, “I do not know”, etc.
- Why so?
- Well, there are many reasons:
- The term andropause does not have the same clear defining characteristics as in menopause
- The andropause initiation stage is less dramatic than menopause
- Andropause can occur at a much wider age range than menopause in women
- Most men are not aware that some of their “aging” symptoms are actually related to the drop-in hormone levels and can be partially corrected with BHRT
- Many men, even if they encounter uncomfortable symptoms related to andropause – hormone decline and imbalance, do not seek medical help…
Now, let us see some of the most common symptoms related to andropause:
- low sex drive
- difficulties getting erections and/or maintaining erections
- lack of energy
- depression
- irritability and mood swings
- loss of muscle strength
- loss of muscle mass
- increased body fat
- hot flashes, etc.
When we talk about ANDROPAUSE, one major male sex hormone that comes to mind, is obviously – Testosterone.
That means after age 45, men should start testing testosterone levels, among other things. Testosterone levels should be measured, even if the patients do not have any obvious hormonal decline or imbalance symptoms.
If Testosterone levels are low correlated to other hormones and the patient does not have any bothersome symptoms, testosterone replacement therapy can be initiated to delay the above-mentioned symptoms and occurrences. This can help maintain their health and well-being.
If a patient presents with some of the symptoms mentioned earlier, a much more comprehensive health assessment needs to be done, and a well-balanced BHRT focused treatment plan needs to be implemented.
One major deficit in assessing hormonal imbalance or deficiency for male patients is that most practitioners focus only on Testosterone.
This is good, but it is not enough!
Healthy men need their progesterone as well. In much more limited, physiological amounts, men need their estrogens too.
Even though this is basic medical science – anatomy and physiology – most practitioners tend to forget that normal structure and functioning of body organs and systems are still part of evidence-based medicine and they should actually be the main focus of most practices as preventive medicine.
The conventional medicine of the last several decades focuses on pathophysiology – abnormal functioning of body parts. And, unfortunately, when doing so, the focus is not on “why” but rather on “what”!
- What does this mean for the patient? – A Superficial approach.
- If the focus would be on “why” the body is malfunctioning-what is causing the malfunctioning, then the practitioner will be able to prepare a better treatment plan for the patient.
- But with the focus on “what” being what are the symptoms of the malfunctioning, the practitioners (most of them) will treat just the symptoms, that will leave the reason those symptoms occurred – unaddressed.
Yet, in mainstream medicine, this is considered evidence based medical practice.
- Who offers the evidence?
- The drug manufacturers.
- Based on what?
- The potential benefits some drugs can have on some symptoms.
Even though, this is an over-simplified scenario, it is very close to the reality of current mainstream medical practice.
I know we deviated from the topic, but we deviated on purpose.
When the topic is hormone related – the evidence-based medicine must stay focused on physiology, not pathophysiology. In this case, a practitioner’s role is to help patients restore/replenish what their bodies lost, with the same thing – BHRT – not something synthetically created that tries to mimic nature unsuccessfully, doing more harm than good along the way.
All that said and hopefully understood, let us get back to testosterone replacement therapy and see why only replenishing the lost testosterone is not only not enough, but it can even be dangerous sometimes.
The proper medical diagnosis for a practitioner to consider testosterone therapy is hypogonadism.
Hypogonadism has been traditionally treated almost exclusively with testosterone supplementation. However, low testosterone can be fairly complex, involving a myriad of factors including:
- the inability of the testes to produce sufficient testosterone,
- improper brain signaling,
- excess estrogen
(Primarily seen as female hormones, estrogens are also very important in men since declining testosterone can alter the androgen – estrogen relationship. While there is not an established target value for the androgen – estrogen ratio, changes in this relationship can result in complications such as declining prostate health).
In some men, clear reasons behind low testosterone can be difficult to determine.
The result, though, can be the same: insufficient testosterone that results in an unhealthy life and is often characterized by symptoms such as loss of libido, erectile dysfunction, depressed mood, and fatigue. After proper diagnosis, including testing for testosterone, estrogen, and luteinizing hormone (LH), properly directed therapy can be dramatically effective in reversing these symptoms and providing a healthier, more robust lifestyle.
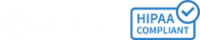
The few diagrams below will take us through the proper assessment steps to help us make the right decision on which treatment combination is best for each patient’s situation.
This will take us back to the understanding physiology. The diagram below illustrates the physiological feedback mechanism in a male gonadal axis:
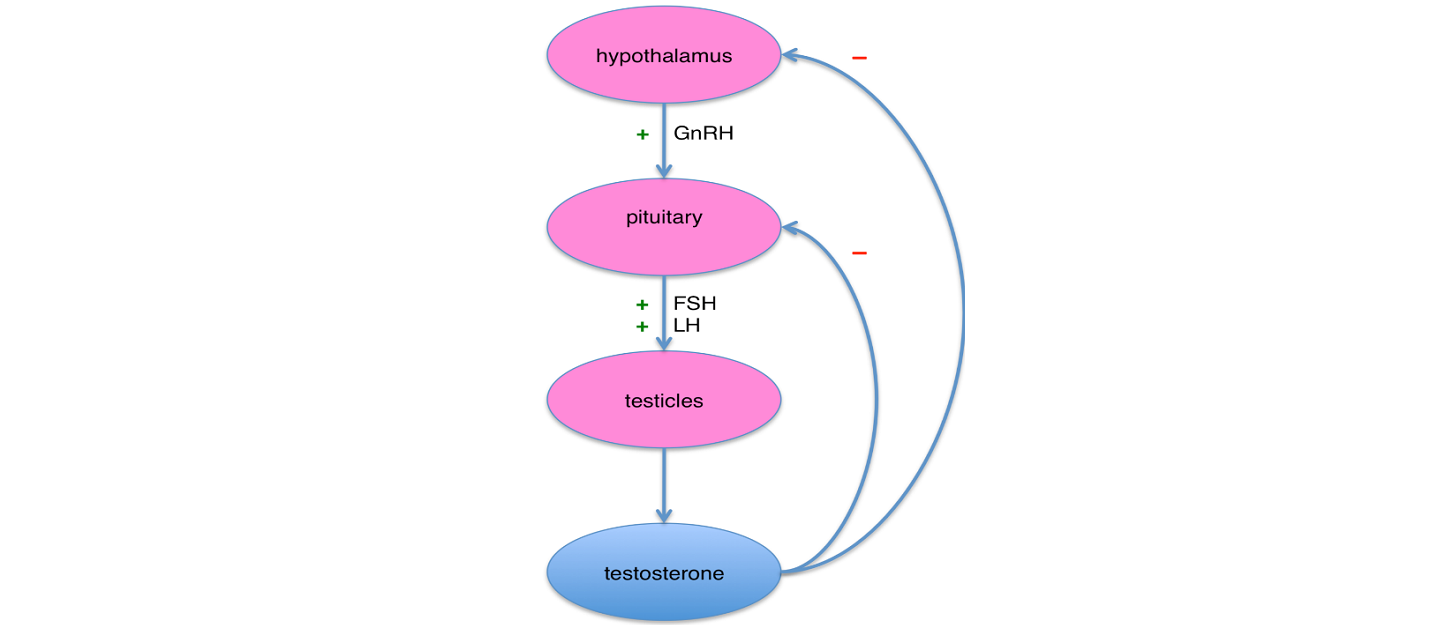
Understanding the hypothalamus/pituitary/gonadal axis and the types of feedback mechanisms, will help us envision the potential wrong directions hormones can take based on other factors that may interfere with in the feedback loops. Creating a treatment plan for hypogonadism should take into consideration: symptoms, lab results, lifestyle factors that affect the feedback mechanism, and has an algorithm based on these findings. (See attached diagram courtesy of PCCA).
Some lifestyle factors and aging can lead to changes in estrogen-androgen ratio that will alter the feedback mechanism, as estradiol is a primary mediator in the HPA axis. Supplementing with testosterone only may lead to more conversion into estrogen that is already in larger amounts than normal. In these cases, an aromatase inhibitor is a better option than testosterone.
High estrogen can also lead high levels of bound testosterone rather than free testosterone.
Anastrozole and letrozole are two of the most commonly used aromatase inhibitors to lower the conversion into estrogen when supplementing with testosterone. To stimulate the endogenous production of testosterone, particularly for patients who desire to stay fertile, HCG or clomiphene may be needed in the treatment plan.
Treatment algorithm for Hypogonadism
We’ll continue in future episodes with dosing recommendations and various forms of testosterone, the pros and cons for each form, etc.
We’ll also talk in more detail about the role of other hormones in men that should be considered in BHRT for men.
Nurten Rasid, MD – Compounding Clinical Consultant @Haldey